Acupuncture Carpal Tunnel Syndrome Relief Confirmed!
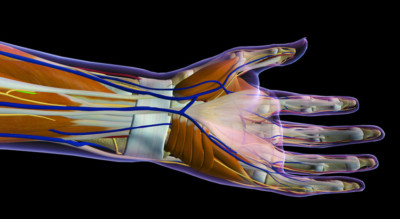 Researchers find acupuncture effective for the treatment of carpal tunnel syndrome (CTS), a local entrapment neuropathy affecting the wrist and hand that causes pain, numbness, and dysfunction. The research team documents acupuncture’s beneficial influence on the morphology of the median nerve and improvement of clinical symptoms.
Researchers find acupuncture effective for the treatment of carpal tunnel syndrome (CTS), a local entrapment neuropathy affecting the wrist and hand that causes pain, numbness, and dysfunction. The research team documents acupuncture’s beneficial influence on the morphology of the median nerve and improvement of clinical symptoms.
According to researchers conducting the investigation, “while previous studies investigated the effect of acupuncture on clinical symptoms and electromyographic studies, to the best of our knowledge, its effect on median nerve morphology was not investigated before.” [1] This study demonstrates that acupuncture influences morphology of the median nerve, which opens up a host of possible future studies that may build upon this foundation of knowledge.
Median nerve compression in the carpal tunnel region of the wrist results in pain, numbness, and tingling in the fingers or hand, as well as possible weakness and atrophy of the hand muscles innervated by the median nerve. [2] More prevalent among women, it is correlated with overuse, diabetes mellitus, rheumatoid arthritis, hypothyroidism, and pregnancy. [3]
Diagnostically and prognostically, musculoskeletal ultrasound imaging has been growing in popularity for monitoring this condition because of its ease and cost effectiveness. Musculoskeletal ultrasound shows the cross-sectional area (CSA) in the wrist level of the median nerve and this study documents correlations between median nerve cross-sectional areas and electrophysiological changes within the CTS affected limb.
A total of 27 female patients (45 limbs) with CTS were diagnosed with electromyographic tests for the purposes of this investigation. The patients were similar in age, BMI (body mass index), duration of disease, and severity of CTS. Exclusionary criteria were the following: radicular pain, polyneuropathy, radial or ulnar nerve diseases, severe CTS, trauma history, prior hand surgery.
In patients with bilateral CTS, both extremities were included in the same group. All patients were informed about the study and provided consent. They were randomly divided into two groups (acupuncture and control). The mean duration of the disease was 18.3 months and 19.3 months respectively. Both groups used night wrist splints for CTS for 4 weeks, while only the acupuncture group received acupuncture treatments. The following nine acupoints were selected for the study:
- Daling (PC7)
- Ximen (PC4)
- Neiguan (PC6)
- Laogong (PC8)
- Qingling (HT2)
- Shenmen (HT7)
- Shaofu (HT8)
- Taiyuan (LU9)
- Quchi (LI11)
The median nerve cross-sectional area was measured at the proximal carpal tunnel with musculoskeletal ultrasound, with the scaphoid and pisiform bones used as bony landmarks for the proximal tunnel where the cross section was measured. [4] Needles of size 0.25 × 25 mm were inserted into the points and were retained for 25 minutes per acupuncture session. Treatments were conducted two or three days per week for four weeks, totaling ten sessions.
Results
The median nerve cross-sectional area was measured by using musculoskeletal ultrasound on the patients while seated and positioned similarly (elbow at 90 degree flexion with the forearm in supination position). Cross-sectional areas of size 9 mm or greater had previously been determined as a possible diagnostic measure for CTS. [5]
Pain severity, hand function, and musculoskeletal ultrasound measurements were taken before and after treatments. The visual analog scale (VAS: 0–10 cm) measured pain severity. The Duruoz Hand Index (DHI) and Quick Disabilities of the Arm, Shoulder and Hand (DASH) scores were used to assess hand functions and disability. All electrophysiological tests were performed by using a Nihon Cohden Neuropack machine.
Compound muscle action potential (CMAP: normal >6.8 mV) measured the reaction of the abductor pollicis brevis muscle to stimulation at the wrist and elbow. Sensory nerve action potential (SNAP: normal >10 uV) measured the reaction of wrist stimulation to signals traveling in the opposite direction of normal signals in the nerve fiber (antidromic) of the second finger. Motor distal latency (normal <3.8 ms), sensory nerve conduction velocity (SNCV: normal >40.4 m/sec), and motor nerve conduction velocity (M-NCV: normal >49.4 m/sec) were also measured before and after treatment.
Acupuncture group positive outcomes proved significant. The median nerve cross-sectional area decreased from 11.6 to10.6 mm, motor distal latency decreased from 4.3 to 4.1 ms, and SNAP increased from 16.7 to17.6 uV. Also in the acupuncture group, VAS decreased from 9 to 4.8, CMAP increased from 12.9 to 14.8 mV, DHI decreased from 47 to 37, Quick DASH decreased from 67.2 to 56.8, S-NCV increased from 31 to 33.2 m/sec, and motor nerve velocity increased from 57.4 to 59 m/sec.
The improvement within the acupuncture group when comparing baseline values with the results highlights the success of acupuncture in decreasing clinical symptoms of CTS. It also highlights its ability to transform median nerve morphology such that acupuncture can reduce the cross-sectional area. The results within the control group were not as significant as the acupuncture group, highlighting the efficacy of acupuncture in treating neuropathic disorders compared with night splint monotherapy.
The researchers cited several investigations showing acupuncture’s positive influence on CTS. Recent studies have used magnetic resonance imaging to show how acupuncture may alter brain activity and the limbic system of CTS patients. [6,7,8] Acupuncture produces anti-inflammatory effects in the median nerve within the carpal tunnel, as well as effects that can be compared to ibuprofen, night splints, and oral or injected steroids. [9,10,11]
Summary
Acupuncture generates beneficial morphological changes in the median nerve of patients with carpal tunnel syndrome and reduces or eliminates symptoms. Based on the scientific evidence, acupuncture is a reasonable treatment option. Consult with a local licensed acupuncturist to learn more.
References:
1 Ural, Fatma Gülçin, and Gökhan Tuna Öztürk. “The acupuncture effect on median nerve morphology in patients with carpal tunnel syndrome: an ultrasonographic study.” Evidence-Based Complementary and Alternative Medicine 2017 (2017).
2. S. Tanaka, D. K. Wild, P. J. Seligman, V. Behrens, L. Cameron, and V. Putz-Anderson, “The US [musculoskeletal ultrasound] prevalence of self-reported carpal tunnel syndrome: 1988 national health interview survey data,”American Journal of Public Health, vol. 84, no. 11, pp. 1846– 1848, 1994.
3. R. J. Spinner, J. W. Bachman, and P. C. Amadio, “The many faces of carpal tunnel syndrome,” Mayo Clinic Proceedings, vol. 64, no. 7, pp. 829–836, 1989.
4. Ural, Fatma Gülçin, and Gökhan Tuna Öztürk. “The acupuncture effect on median nerve morphology in patients with carpal tunnel syndrome: an ultrasonographic study.” Evidence-Based Complementary and Alternative Medicine 2017 (2017).
5. J. T. Mhoon, V. C. Juel, and L. D. Hobson-Webb, “Median nerve ultrasound as a screening tool in carpal tunnel syndrome: correlation of cross-sectional area measures with electrodiagnostic abnormality,” Muscle and Nerve, vol. 46, no. 6, pp. 871–878, 2012.
6. A. U. Asghar, G. Green, M. F. Lythgoe, G. Lewith, and H. MacPherson, “Acupuncture needling sensation: the neural correlates of deqi using fMRI,” Brain Research, vol. 1315, pp. 111–118, 2010.
7. V. Napadow, J. Liu, M. Li et al., “Somatosensory cortical plasticity in carpal tunnel syndrome treated by acupuncture,” Human Brain Mapping, vol. 28, no. 3, pp. 159–171, 2007.
8. V. Napadow, N. Kettner, J. Liu et al., “Hypothalamus and amygdala response to acupuncture stimuli in carpal tunnel syndrome,” Pain, vol. 130, no. 3, pp. 254–266, 2007.
9. M. Hadianfard, E. Bazrafshan, H. Momeninejad, and N. Jahani, “Efficacies of acupuncture and anti-inflammatory treatment for carpal tunnel syndrome,” Journal of Acupuncture and Meridian Studies, vol. 8, no. 5, pp. 229–235, 2015.
10. Ho, Chien-Yi, Hsiu-Chen Lin, Yu-Chen Lee, Li-Wei Chou, Ta-Wei Kuo, Heng-Wei Chang, Yueh-Sheng Chen, and Sui-Foon Lo. “Clinical effectiveness of acupuncture for carpal tunnel syndrome.” The American journal of Chinese medicine 42, no. 02 (2014): 303-314.
11. Yang, Chun-Pai, Nai-Hwei Wang, Tsai-Chung Li, Ching-Liang Hsieh, Hen-Hong Chang, Kai-Lin Hwang, Wang-Sheng Ko, and Ming-Hong Chang. “A randomized clinical trial of acupuncture versus oral steroids for carpal tunnel syndrome: a long-term follow-up.” The Journal of Pain 12, no. 2 (2011): 272-279.

 The first prescription medication extracted from the marijuana plant is poised to land on pharmacists’ shelves this fall. Epidiolex, made from purified cannabidiol, or CBD, a compound found in the cannabis plant,
The first prescription medication extracted from the marijuana plant is poised to land on pharmacists’ shelves this fall. Epidiolex, made from purified cannabidiol, or CBD, a compound found in the cannabis plant,


